Callus Foot
calluses on bottom of feet are tough, thickened skin that form on the surface of sole of your foot.
Calluses are extremely common. They’re not a cause for concern unless certain problematic symptoms arise alongside them especially with diabetic sensory loss
Cause–
Calluses develops due to repeated friction, irritation, or pressure hence are most often found on sole of foot which support our body weight, because of poorly fitting footwear and frequent walking.
Any skin selected part if exposed to excess friction over a long period of time can cause callus
Calluses form as a natural reaction for protection for the plantar skin against this pressure or too much friction. Otherwise will cause a blister or abrasion instead
Locations on Feet –
On the foot, calluses locations on sole of foot are typically form on the
balls of the foot (metatarsal-phalangeal joint area),
toe tips
compression applied by tightly fitting shoes or high heel shoes with thin socks or no socks are often liable to excess pressure to the foot
callus are dead cells nothing but the accumulation of undifferentiated keratinocytes in the outer layer of skin,
High levels of activity, especially people who put pressure on the feet, also can contribute to plantar calluses. Runners and athletes, for instance, or those that walk rather than drive is more susceptible to plantar calluses.
There’s evidence that smoking can increase the likelihood of developing calluses on the feet. this is often thought to flow from to the constriction of vessels within the extremities that’s caused by smoking. this will cause the decline or atrophy of the subcutaneous tissue. Eventually, this might cause increased contact between bone and skin, creating more calluses.
Bone deformities also can be responsible.
Sometimes, a bone deformity will end in excess pressure being applied to certain areas of the foot, especially if a person’s gait is altered as a result of the deformity.
Clinical Presentation-The skin of a callus foot is yellowish or grey or black. The skin will be felt as hard, rough, dry, and flaky. On direct pressure while walking it may be painful on later stages.
Differentiating between corn and plantar wart
If you are unsure what you developed a corn or a wart on your sole of foot, rather than a callus.
A corn may be a small patch of thickened skin with an inverted cone like plug in the center.
Corns seen commonly on the tops and side of the toes.
Plantar warts, on the opposite hand, are often found on bottom of the foot.
Warts have a cauliflower-like appearance, with small black pinpoints within the center. A wart may bleed once you walk thereon.
Plantar warts don’t have skin striations (engraved grooves) once they develop on the foot. Plantar warts are most painful when side-to-side pressure is applied, while plantar calluses can cause pain when direct pressure is applied to the world.
- Your callus features a clear fluid or pus discharge.
this is often a symbol that the callus is infected or ulcerated and wishes immediate treatment.
• usually plantar calluses are recurring unless customized footwear used or pressure offloading surgery done for that area.
• If you notice that your callus is red, particularly even on touch painful. These symptoms suggestive of infection.
How is plantar callus treated?
Most plantar calluses are often treated as outpatient in clinics. Soaking your feet in warm water for a minimum of ten minutes, and using thick moisturizers and lotions once the skin is dry can help soften the callus. you’ll also use pumice stones or metal files to reduce the callus. This treatment is best after soaking your feet in warm water.
Shoe pad custom inserts and shoes with more support and cushioning would relieve pressure on problem areas.
If home treatments aren’t effective, a foot doctor can assist you treat your plantar callus.
Your foot doctor has two methods of treating calluses. the primary is to get rid of the skin of the callus with a scalpel.
The second is to use patches or creams containing 40% salicylic acid to the callus. The latter is best when reapplied daily, and when it’s used after employing a pumice or metal file to get rid of the callus.
To prevent plantar calluses in future , your foot doctor may advise you to wear a special sort of shoe that’s better suited to your foot shape and foot arch. they’ll even be ready to check out your gait and determine if that’s why you develop calluses.
If a bone deformity is causing the callus, your foot doctor can recommend surgery to correct it.
Plantar calluses are extremely common among people of all ages. If the callus isn’t affecting how you walk or showing symptoms of an infection, it’s not a cause for concern.
In most cases, home treatments should assist you manage them.
If you’re experiencing regular plantar calluses within the same place, ask your doctor to seek out why.
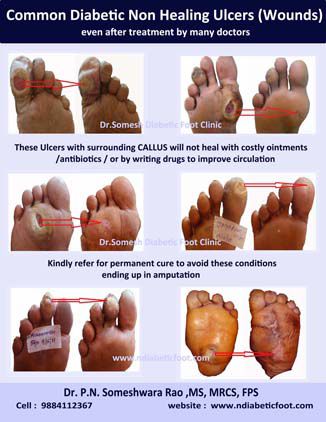
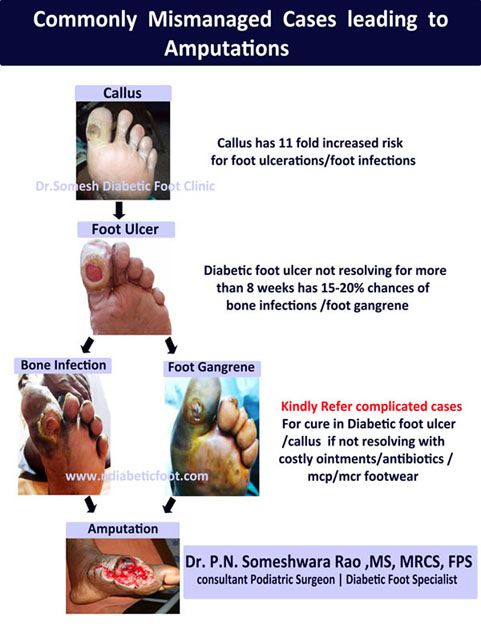
Complications
in initial stages calluses are not harmful although mild discomfort will be felt,
person with intact sensation when it is very hard tries to avoid walking over callus to avoid pain causing more stress on normal side causing gait walking disturbance leading to knee and back pain later stages brisk walking or jogging with rubbing callus forcefully over ground can cause blisters, and infection.
In diabetic persons with neuropathy due to muscle loss and increased pressure at bony prominences callus formation occurs, capillary refilling is delayed after many years of diabetes, once callus compresses skin while doing brisk walking or excessive frequent rubbing of callus over skin the tiny blood vessels which feed skin it deprives skin of its nutrients not allowing capillary refilling to happen if it is prolonged for certain period of time , creates blister or infection or ulcerations.
Callus is an early sign of diabetic foot ulceration and infection that can happen if not proper care given in the initial stages, or can turn into gangrene needing amputation.
If ulcer is already developed , callus ulcer when grown very hard can tear tiny blood vessels on shear friction and pressure , which can present as bleeding which patient notices as they walk in their homes drops of blood on the floor , once blood is outside surfaces it can act as a portal for bacteria to get into body and infection starts.
If there is no ulcer callus on friction and pressure to tiny vessels can turn them to hematoma formation and it gets turned into pus formation and gangrene progression happens, callus nonhealing ulcers turning into diabetic foot infections are leading cause of diabetic foot amputations.